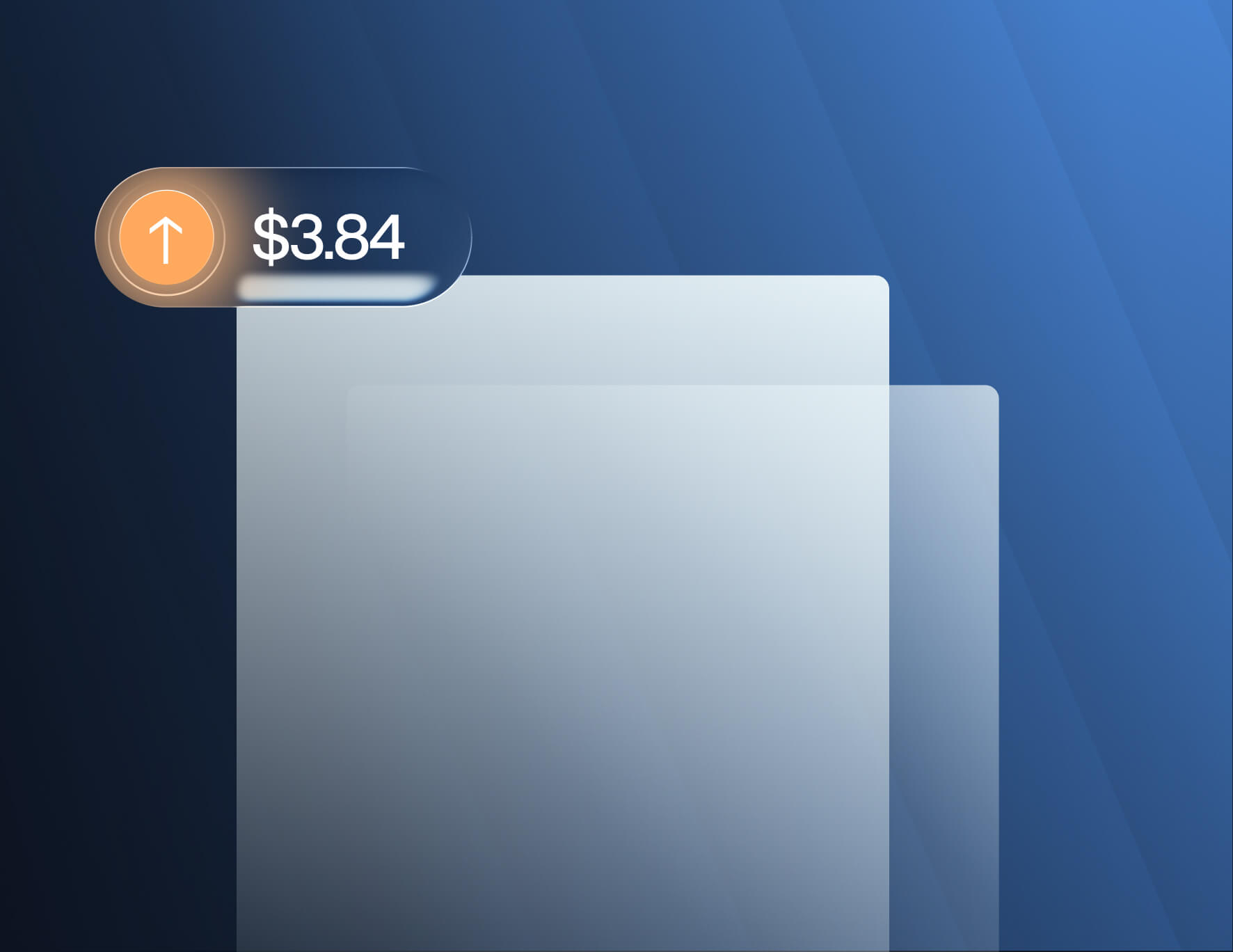
In Notice 2025-61, the IRS announced an increase to the Patient-Centered Outcomes Research Institute (PCORI) fee for plan years ending on or after Oct. 1, 2025, and before Oct. 1, 2026.
The new applicable dollar amount is $3.84 per covered life, up from $3.47 for plan years ending between October 2024 and October 2025.
Understanding the PCORI Fee
The PCORI fee was created under the Affordable Care Act to fund research on the comparative effectiveness of medical treatments, helping patients, providers, and policymakers make evidence-based healthcare decisions.
Originally scheduled to expire in 2019, the Further Consolidated Appropriations Act of 2020 extended the PCORI fee through plan years ending before Sept. 30, 2029.
Employers subject to the fee must file IRS Form 720, Quarterly Federal Excise Tax Return, and remit payment by July 31 following the end of the plan year.
The PCORI fee applies to:
- Issuers of specified health insurance policies under IRC § 4375.
- Plan sponsors of self-insured health plans under IRC § 4376.
Both use the same formula:
- Average number of covered lives × Applicable dollar amount
For the 2026 filing season, that means multiplying total covered lives by $3.84.
Example
If an employer-sponsored self-insured plan covers 1,000 lives during a plan year ending Dec. 31, 2025, the PCORI fee due by July 31, 2026, would be:
- 1,000 × $3.84 = $3,840
Filing Deadlines & Procedures
Employers with calendar-year plans (ending Dec. 31) must:
- File Form 720 by July 31, 2026.
- Use the second-quarter form (due at the end of July).
- Record payment under “Patient-Centered Outcomes Research Fee.”
The IRS does not provide extensions for PCORI fee filing or payment.
Compliance Implications for Employers
While the PCORI fee may seem minor compared to broader ACA compliance obligations, failure to file or pay can result in IRS penalties and interest. Employers should:
- Confirm who is responsible for filing (the carrier for fully insured plans; the plan sponsor for self-insured plans).
- Review plan documents to determine plan year-end dates.
- Coordinate with payroll and accounting teams to ensure fees are calculated and submitted accurately.
- Maintain audit-ready documentation in case of IRS inquiries.
Get Help With ACA Compliance
Trusaic’s ACA Compliance Solution ensures streamlined reporting. Track, file, and furnish 1095-C and 1094-C forms while minimizing penalty risks.
ACA Complete® delivers everything you need to track, prepare, furnish, and file 1095-C forms and defend your ACA compliance.
- Monthly monitoring: get alerts when offers of coverage are required
- Designated ACA specialist: expert support at your service
- Penalty risk assessment: identify coverage gaps and address liabilities
Schedule a demo now to see how we can assist you with your ACA compliance for the 2026 filing season.